The Lifecycle of HMPV | How the Virus Infects and Spreads
Human Metapneumovirus (HMPV) is a respiratory pathogen that is often overshadowed by other viruses such as influenza or RSV (Respiratory Syncytial Virus). Yet, HMPV has a significant impact on global health, particularly among infants, older adults, and individuals with weakened immune systems. To understand how this virus operates, let’s dive into its lifecycle, exploring how it infects and spreads.
The Problem: Why Understanding HMPV Matters
Respiratory illnesses are among the leading causes of hospitalization worldwide. HMPV is a major player in this category, contributing to acute respiratory infections (ARIs). Studies show that it’s responsible for 5-10% of respiratory illnesses in children and adults. Despite its prevalence, awareness about HMPV remains limited.

Failing to understand the mechanisms behind how HMPV spreads and infects can lead to delayed diagnoses, ineffective infection control measures, and ultimately, higher healthcare burdens. This knowledge gap is where we need to focus attention.
The Agitation: The Growing Burden of HMPV
The first human metapneumovirus was identified in 2001, but retrospective analyses reveal it has been circulating in humans for decades, possibly centuries. The virus is particularly concerning because:
1. Seasonal Epidemics: HMPV cases typically peak during late winter and early spring, overlapping with RSV and influenza seasons. This creates diagnostic challenges and often leads to co-infections.
2. High-Risk Groups: Children under the age of 5, elderly individuals, and immunocompromised patients are disproportionately affected. In children, HMPV is a leading cause of bronchiolitis, second only to RSV.
3. Healthcare Strain: Studies estimate that HMPV leads to 20,000 hospitalizations annually in the U.S. alone, with considerable costs associated with its treatment and management.
Understanding the lifecycle of HMPV is critical for developing better prevention, diagnosis, and treatment strategies.

The Solution: Exploring the Lifecycle of HMPV
Step 1: Entry into the Host
- HMPV is primarily transmitted through respiratory droplets or direct contact with contaminated surfaces. Like many respiratory viruses, its entry begins in the upper respiratory tract, specifically targeting epithelial cells in the nose, throat, and lungs.
Mechanisms of Entry
HMPV attaches to host cells via its glycoproteins, primarily the F protein (fusion protein). This protein plays a pivotal role in:
– Attachment: HMPV binds to the surface receptors of epithelial cells, such as heparan sulfate proteoglycans.
– Fusion: The F protein facilitates the fusion of the viral envelope with the host cell membrane, allowing the virus to release its RNA genome into the cell.
Case Study Insight
A 2019 study published in The Journal of Virology highlighted how modifications in the F protein could alter the virus’s infectivity. Researchers noted that even small mutations in this protein impacted how efficiently HMPV could enter host cells, offering potential targets for antiviral therapies.
Step 2: Replication Inside the Host Cell
Once inside, the viral genome, a single-stranded RNA molecule, hijacks the host’s machinery to replicate and produce new viral particles.
HMPV is a negative-sense RNA virus, meaning its genome must first be transcribed into a complementary positive-sense RNA strand before translation can occur. The virus relies on its RNA-dependent RNA polymerase to perform this task.
– Transcription: Viral RNA polymerase transcribes the genome into messenger RNA (mRNA).
– Translation: Host ribosomes translate the mRNA into viral proteins, such as structural proteins (N, P, L) and glycoproteins (F, G).
Viral Assembly
After replication and translation, the newly formed viral RNA and proteins assemble into complete virions within the host cell’s cytoplasm.
Cellular Impact
During this stage, the infected cells often show signs of cytopathic effects (CPE), such as syncytia formation. Syncytia are large, multinucleated cells formed by the fusion of adjacent infected cells.
Case Study Insight
A 2020 observational study found that patients with severe HMPV infections had higher rates of syncytia formation, correlating with increased viral loads and more severe respiratory symptoms.
Step 3: Viral Release
Once new virions are assembled, they exit the host cell to infect neighboring cells.
Methods of Release
– Exocytosis: Virions are released without destroying the host cell, allowing the infection to continue stealthily.
– Cell Lysis: In severe cases, the host cell bursts, releasing large quantities of virions into the respiratory tract.

Immune Evasion
HMPV employs strategies to evade the host’s immune response during this phase. For example:
– It suppresses the production of interferons (key antiviral proteins).
– It alters the host’s immune signaling pathways to delay detection.
Step 4: Spread Within the Host
After being released, HMPV spreads to lower respiratory tract regions, such as the bronchi and alveoli. This progression often results in:
– Bronchiolitis (inflammation of the small airways).
– Pneumonia in severe cases.
Step 5: Transmission to Others
HMPV spreads from person to person through:
– Respiratory droplets: Sneezing, coughing, or talking.
– Fomites: Contaminated surfaces like doorknobs and toys.
Environmental Stability
HMPV can survive on surfaces for several hours, increasing its transmission potential in shared spaces like schools and healthcare settings.
Case Study Insight
An investigation during an outbreak in a long-term care facility revealed that surface disinfection and hand hygiene significantly reduced HMPV transmission rates.
Conclusion: Breaking the Cycle
Understanding the lifecycle of HMPV gives us actionable insights into combating the virus. For instance:
1. Prevention: Focused efforts on surface disinfection, mask usage, and hand hygiene can break the chain of transmission.
2. Early Detection: Improved diagnostic tools, such as PCR-based tests, can identify HMPV early in patients, leading to better outcomes.
3. Treatment Development: Targeting the F protein or RNA polymerase could yield effective antiviral therapies.
HMPV is not just another respiratory virus. It is a complex pathogen with unique characteristics that demand our attention. By understanding how it infects and spreads, we can take meaningful steps toward reducing its impact on global health.
In this fight against HMPV, knowledge is our most powerful weapon. Let’s use it wisely.
1. Prevention: Focused efforts on surface disinfection, mask usage, and hand hygiene can break the chain of transmission.
2. Early Detection: Improved diagnostic tools, such as PCR-based tests, can identify HMPV early in patients, leading to better outcomes.
3. Treatment Development: Targeting the F protein or RNA polymerase could yield effective antiviral therapies.
HMPV is not just another respiratory virus. It is a complex pathogen with unique characteristics that demand our attention. By understanding how it infects and spreads, we can take meaningful steps toward reducing its impact on global health.
What We Do The HMPV Case in a Company Employee What was the Awareness to other employee??
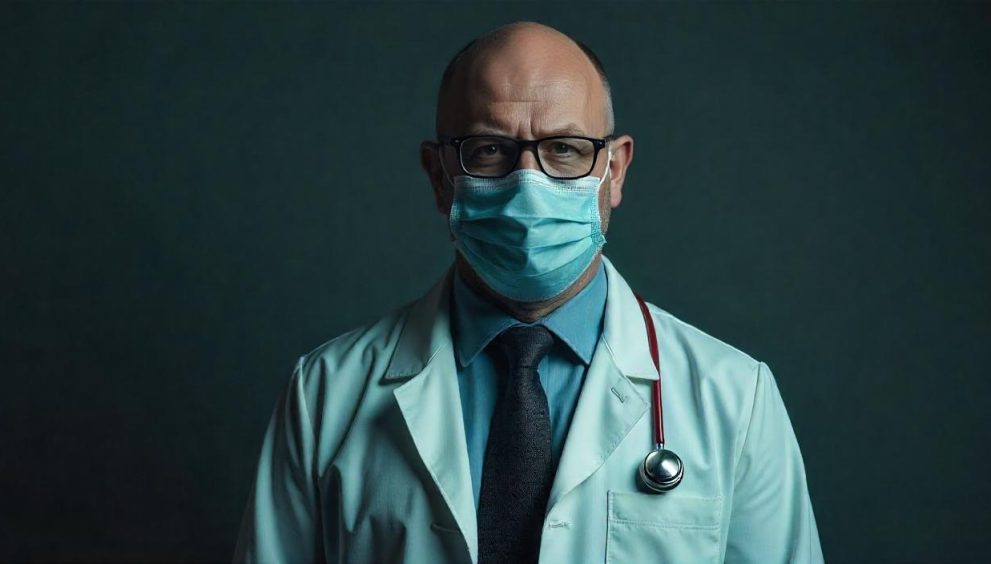
When a company employee is diagnosed with Human Metapneumovirus (HMPV), it’s crucial to raise awareness among other employees to prevent the spread of the virus. Here’s how it can be done in a human and relatable way:
- Immediate Communication: Inform all employees about the case promptly, ensuring confidentiality and sensitivity. Explain what HMPV is, its symptoms (like cough, fever, and congestion), and how it spreads (through respiratory droplets).
- Educational Sessions: Organize informational sessions or distribute materials about HMPV, its symptoms, and preventive measures. This can include posters, emails, or even short videos.
- Promote Hygiene Practices: Encourage regular handwashing, using hand sanitizers, and disinfecting shared surfaces. Provide hand sanitizers and disinfectant wipes around the workplace.
- Encourage Sick Employees to Stay Home: Make it clear that employees feeling unwell should stay home to recover and avoid spreading the virus. Offer flexible sick leave policies if needed.
- Implement Preventive Measures: Encourage wearing masks, especially in crowded areas, and maintaining physical distance. Improve ventilation in the workplace to reduce the risk of airborne transmission.
- Regular Updates: Keep employees informed about any new cases or updates regarding HMPV in the workplace. Transparency helps build trust and ensures everyone is on the same page.
what was the significant of HMPV ??
- Mild Symptoms for Most: For most people, HMPV causes symptoms similar to a common cold, like a runny nose, cough, and mild fever. These symptoms usually resolve on their own within a few days.
- Risk for Vulnerable Groups: While most people recover easily, HMPV can be more serious for young children (especially those under five), older adults, and people with weakened immune systems. In these groups, it can lead to more severe respiratory infections like pneumonia or bronchiolitis.
- Seasonal Occurrence: HMPV is most active during the winter and spring months, similar to the flu. This means that outbreaks are more common during these times.
- Prevention is Key: There’s no specific treatment or vaccine for HMPV, so prevention is crucial. This includes regular handwashing, avoiding close contact with sick individuals, and practicing good hygiene.
- Global Presence: HMPV has been around for decades and is found worldwide. Most people have been infected with it by the time they are five years old and can catch it again throughout their lives.
In this fight against HMPV, knowledge is our most powerful weapon. Let’s use it wisely.
 English
English 













